Sinus, Allergy, or Migraine headache? 2024
The maxillary sinuses are located behind the checks on either side of the face. They are innervated by the 2nd division of the trigeminal nerve, called the maxillary nerve. The maxillary nerve supplies the nose, cheeks, and the upper part of the lips. The maxillary sinuses are often involved with allergic rhinitis and are a frequent site for migraine headache.
This is an article by Britt Talley Daniel MD, member of the American Academy of Neurology, the American Headache Society, migraine textbook author, and blogger.
As a general rule there is no legitimate “Sinus or allergy headache.” Sinus headache was created in the fifties to sell pseudoephedrine, a mild nasal vasoconstrictor and a decongestant. The words “allergy” and “sinus headache” are not mentioned in the International Classification of Headache-V3. Allergy symptoms can aggravate migraine attacks but they are separate medical conditions.
Currently there are over 200 pseudoephedrine type drugs in the United States. “Sinus headache” is not found in any other country in the world except the US, and is an inaccurate medical term which usually denotes migraine headache.
Allergic rhinitis can aggravate migraine if the patient is stressed or ill from allergic symptoms. Allergic rhinitis is an aggravating factor relating to migraine, but a separate medical issue. Patients with allergic rhinitis may not sleep well and poor sleep is a migraine trigger.
There is no allergy headache, and allergic symptoms can aggravate migraine indirectly, but there is no direct allergic pathophysiologic mechanism causing headache. An allergic reaction is an antigen-antibody reaction, where the antigen is a foreign protein like cedar pollen, and an antibody is another complex protein made by mast cells in the immune system to combat the invasion. In the process Gamma E is released.
Many different chemicals cause vasodilation and therefore aggravate migraine headache. This is why MSG, chocolate, tyramine in aged cheese, and nitrates in hot dogs may aggravate migraine. There is a relationship between the ingestion of such a chemical and headache, but the headache comes because of vasodilation caused by the offending chemical (i.e. chocolate) not from an allergic reaction.
Allergic rhinitis is the proper name for the lay terms of “sinus,” “allergies,” or “hay fever.”
The diagnosis off allergic rhinitis is based on a history of seasonal or continuous symptoms of nasal and ocular itching, sneezing, nasal stuffiness, nasal drainage, and cough. It is usually familial. The diagnosis can be confirmed by demonstration of IgE antibodies by either skin testing or radioallergosorbent testing (RAST). Skin testing is preferred because of greater sensitivity and decreased cost.
Related questions.
1.How is “sinus headache” related to migraine?
Cady, et al published a paper, Sinus Headache: A Neurology, Otolaryngology, Allergy, and Primary Care Consensus on Diagnosis and Treatment in the Mayo Clinic proceedings in 2005. (Mayo Clin Proc. 2005;80(7):908-016.) This paper was regarding headache in the sinus area and migraine and the discussion centered around how “sinus headache” is usually migraine.
Dr. David Dodick, head of the section of headache at the Mayo Clinic published The Sinus, Allergy and Migraine Study (SAMS) in Headache, 2007 Feb;47(2):213-224). This was an article regarding 100 patients with a self-diagnosis of “sinus headache.” He found 97 of the 100 patients had a diagnosis of migraine alone or migraine with medication overuse headache. The conclusion of this report was:
“The majority of those with self-diagnosed sinus headache have migraine or probable migraine. In those patients with migraine, the most common reasons for misdiagnosis include headache triggers, pain location, and associated features ("guilt by provocation, location, and association") commonly attributed to sinus headache. The clinician must be aware of these unique presentations of migraine so that a correct diagnosis can be made and effective treatment instituted. A portion of patients with self-diagnosed sinus headache suffer from a headache type, which is unclassifiable by the current IHS criteria. These headaches are characterized by bilateral maxillary pressure, mild to moderate pain intensity, cranial autonomic symptoms, and the complete absence of migraine features.”
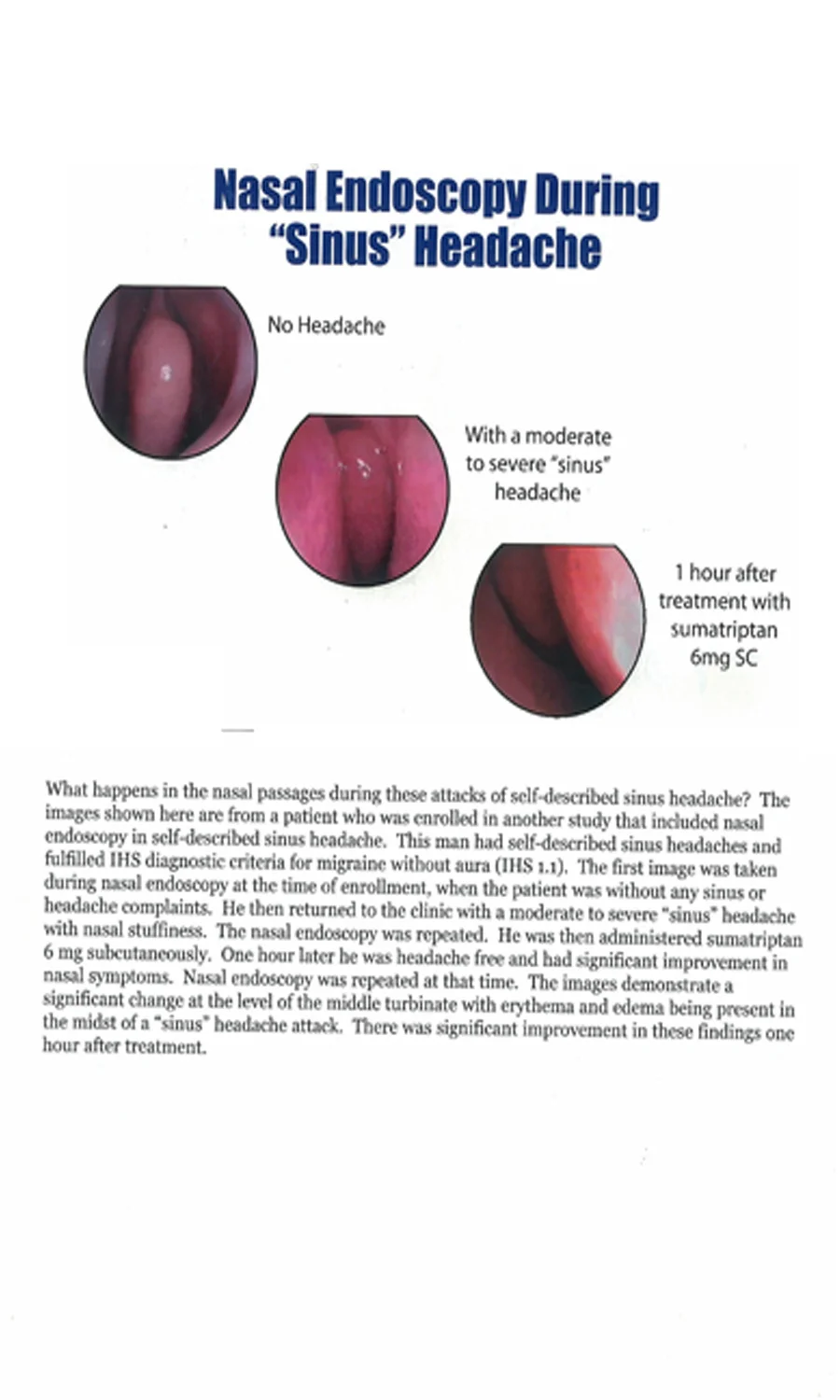
Migraine causes vasodilatation of the cerebral and nasal arteries. This is part of the migraine process. Dilatation of nasal arteries causes congestion or a “stopped up” feeling in the nose. There maybe headache with the nasal congestion and TV ads teach treatment of the symptoms with something like Sine-aid, or Advil Sinus. These drugs have pseudoephedrine in them which is a mild vasoconstrictor; and also there is a mild over-the-counter analgesic, so the patient’s “sinus headache” gets a little better.
2. How is acute rhinosinusitis diagnosed?
Diagnostic criteria:
A. Any headache fulfilling criterion C
B. Clinical, nasal endoscopic and/or imaging evidence of acute rhinosinusitis
C. Evidence of causation demonstrated by at least two of the following:
1. headache has developed in temporal relation to the onset of the rhinosinusitis
2. either or both of the following:
a) headache has significantly worsened in parallel with worsening of the rhinosinusitis
b) headache has significantly improved or resolved in parallel with improvement in or resolution of the rhinosinusitis
3. headache is exacerbated by pressure applied over the paranasal sinuses
4. in the case of a unilateral rhinosinusitis, headache is localized ipsilateral to it
D. Not better accounted for by another ICHD-3 diagnosis.
3. How is “sinus headache” treated.
First, one must understand that the phrase “sinus headache” is an inaccurate term since it usually relates to migraine and the better question would be “How is frontal maxillary sinus located migraine treated.”
Without proper education, here is how “sinus headache” treatment plays out. The patients thinks: “I had a sinus headache. I took sinus medication and the headache got a little better.” No, the patient really had a migraine and they treated with a vasoconstrictor, pseudoephedrine, and the headache got a little better.
This headache would have been better treated at onset with one of the 7 triptans, since 80% of persons who treat with a triptan are headache free in 2 hours. A pseudoephedrine treated patient will usually not do so well, and there is the risk that if the patient is unlucky and keeps taking pseudoephedrine for a few days along with their usual dose of 4 cups of coffee (135X4=540 mg caffeine) they may continue with daily headache and develop medication overuse headache. The migraine lifestyle calls for the migraine patient to be off daily caffeine.
Triptans are the best drugs for acute treatment of migraine and 80% of patients may be headache free if treated at onset with a triptan, the type of rapid, effective migraine treatment that the pseudoephedrine using patient only dreams of.
The usual maxillary sinus, cheek headache medical problems are frontal migraine without aura or acute rhinosinusitis. Patients with allergic rhinitis may have nasal congestion, tearing, sneezing, or clear nasal fluid production.
To have a diagnosis of acute rhino sinusitis the patient should have frontal headache, nasal congestion, nasal discharge of pus of a green of a dark yellow color. To clench the diagnosis the doctor should order a Sinus CAT scan, to confirm pus in the maxillary sinus. In Dr. Dodick’s study, mentioned above on Sinus headache, there were 3 scans showing maxillary pus and 97 normal scans for the migraine patients.
4. How is Allergic Rhinitis treated?
Allergic rhinitis with clear nasal discharge
Treatment of allergic rhinitis is stepwise with antihistamines as the first step followed by nasal steroids, decongestants, and anticholinergics. Immunotherapy (allergy shots) can be introduced if the patient fails to respond or cannot tolerate medication.
Older antihistamines like Benadryl (Diphenhydramine) are available over-the-counter, but are commonly very sedating and therefore poorly tolerated. Benadryl is commonly appended to over the counter analgesics like Tylenol or Advil and sold as treatment of insomnia with names of Tylenol PM and Advil PM which is just Tylenol and Benadryl and Advil and Benadryl.
Current newer antihistamines are:
Claritin (loratadine)
Zyrtec (cetirizine)
Allegra (fexofenadine)
Dimetane (rompheniramine))
Trimeton (chlorpheniramine)
Tavist (clemastine)
Common nasal steroids are Flonase, Nasocort, and Rhinocort
Pseudoephedrine is a decongestant and not an antihistamine, and it may be added orally when nasal steroids and antihistamines are inadequate. Claritin, for example, comes as Claritin D, which has pseudoephedrine added as a decongestant. Topical agents such as Afrin nose spray should only be used for several days because overuse can lead to rebound congestion and rhinitis medicamentosa. Patients with severe symptoms should consider allergy referral for immunotherapy (allergy shots).
The International Classification of Headache Disorders (ICHD) 3-Beta states: “The term “sinus headache” is outmoded because it has been applied both to primary headaches and headache supposedly attributed to various conditions involving nasal or sinus structures.”
Primary headaches are Migraine and Tension Type Headache. This whole area of frontal migraine and rhinosinusitis is difficult to read and clinically to sort out, so I’m going to include the official statements from ICHD-3:
5. What does ICDH-3 say about Sinus Headache?
“Clinical evidence of acute rhinosinusitis may include purulence (pus) in the nasal cavity, nasal obstruction, hyposnia/anosmia and/or fever. Chronic sinusitis is generally not validated as a cause of headache or facial pain unless relapsing into an acute stage. Migraine and tension-type headache are often confused with headache committed to rhinosinusitis because of similarity location of the headache.
A group of patients can be identified who have of all the features of migraine without aura and additionally, concomitant clinical features such as facial pain, nasal congestion and headache triggered by weather changes. None of these patients have purulent nasal discharge or other features diagnostic of acute rhinosinusitis. Therefore, is necessary to differentiate headache attributed to rhinosinusitis from so-called "sinus headaches", a commonly made but nonspecific diagnosis. Most such cases fulfill the criteria for migraine without aura with headache either accompanied by prominent autonomic symptoms in the nose or triggered by nasal changes.”
If you don’t have the above listed symptoms and clinical findings, then you don’t have acute rhinosinusitis. Patients with what they call “sinus headache” usually localize the pain to behind the eyes, the forehead, or the cheeks. The American Academy of Neurology has said that most patients with what they call “sinus headache” have a diagnosis of migraine made by a neurologist. Many of these patients have no purulent nasal discharge which is a cardinal requirement of true nasal sinusitis, an infection in the sinus areas.
6. What does the media and especially TV ads say about Sinus Headache?
Old Dristan Ad for Sinus headache
The myth about sinus headache has been taught to the American public since the 1950s by erroneous advertising such as Tylenol sinus ads on TV. This misconception doesn’t exist in Europe where no one has heard of “sinus headache.”. It is a marketing idea made up in America to sell pseudoephedrine type drugs to the unwary consumer. It is common to have more than one type of migraine headache. Many persons accurately name their worst, often one-sided headaches as migraines, but they are not aware that their milder, front of the head “sinus headache” may be migraine too.
7. Can migraine produce sinus like symptoms?
During the migraine process the cranial arteries dilate, a process called vasodilation. With a frontal migraine in the sinus areas, the arteries in the nasal turbinates, the vascular tissue in the depth of the nose, dilate and the patient notices nasal congestion which is a migraine symptom. Sinus headache TV ads would say nasal congestion is due to a “sinus” problem.
Patients with acute rhinosinusitis should have green or yellow frontal nasal discharge as evidence of infection, not a clear watery discharge like with allergic rhinitis.
8. Does Pseudoephedrine really work for Sinus headache, meaning does it work for mild migraine headache?
Pseudoephedrine causes vasoconstriction of nasal turbinate arteries and is therefore is a “weak” migraine drug, like caffeine. Pseudoephedrine is a mildly effective over the counter drug for acute migraine. Today there are over 200 pseudoephedrine drugs in the U.S. The “sinus headache” myth is driven by big pharma to sell pseudoephedrine drugs. Pseudoephedrine is also spelled “Sudafed.” Pseudoephedrine has been banned for importation to the U.S. by the FDA.
9. Pseudoephedrine and methamphetamine.
Ten years ago in Dallas there was an article in the Dallas Morning News about a man who went into Eckerd’s drug store, now CVS, and bought $5000 worth of pseudoephedrine. The alert pharmacist knew what was going on and called the cops who picked him up in the CVS parking lot and went to his house, where they found a “meth lab” he was planning to make from the pseudoephedrine and sell to school children in Garland, Texas. He ended up in jail. The Wall Street Journal had an article about a man who made a “meth lab” in the men’s room of Laguardia airport in New York.
10. What’s the problem with Methamphetamine?
Methamphetamine addiction is a big problem in America and methamphetamine comes from pseudoephedrine. When I got my medical license to practice medicine in Texas in 1970 pseudoephedrine was doctor’s prescription only but then it went over the counter. Now in Texas someone who buys pseudoephedrine at the drug store has to register their driver’s license, while in Oklahoma it is illegal, and Utah has it as prescription only.
How about this statement? It’s tough but it’s true. The phrase “sinus headache” is made and marketed by a mafia driven drug industry in the United States to sell--pseudoephedrine.
In November 2018 the Wall Street Journal reported that methamphetamine use caused the most drug related deaths in America, just for that one month, instead of the usual cause--opioid narcotics.
This site is owned and operated by Internet School LLC, a limited liability company headquartered in Dallas, Texas, USA. Internet School LLC is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. Although this site provides information about various medical conditions, the reader is directed to his own treating physician for medical treatment.
All the best.
Follow me at: www.doctormigraine.com, Pinterest, Amazon books, Podcasts, and YouTube.
Britt Talley Daniel MD